We will examine multiple theories on the structure and function of Qi and the acupuncture meridians themselves. The end result is an expanded conceptual understanding of the meridian system and the Qi that flows through it. This will result in a greater understanding of what we are accomplishing with our treatments and the importance of providing acupuncture and chiropractic together.
Acupuncture: Structural Meridian Concepts
I. what is Qi?
A. Defined even in Ancient China as ‘Life Force’
B. Examples: light, electrons, food, sunlight
C. believed to permeate everything and connect us and our environment
II. Meridians
A. 14 main meridians
B. 361 main points
C. Qi constant, balanced flow through them
III. The search for the elusive Meridians
A. Commonly accepted view: electrical low resistance points
1. easily measurable for some time now with instruments
2. in fact, this is the basis for using microcurrent for point identification
3. There have been electrical changes noted with acu point stimulation
B. Photons also measured
1. Measurable change with photon emission with acu point stimulation can be demonstrated experimentally
2. equipment is more sophisticated
3. more complex experimental design needed
4. Non visible light spectrum
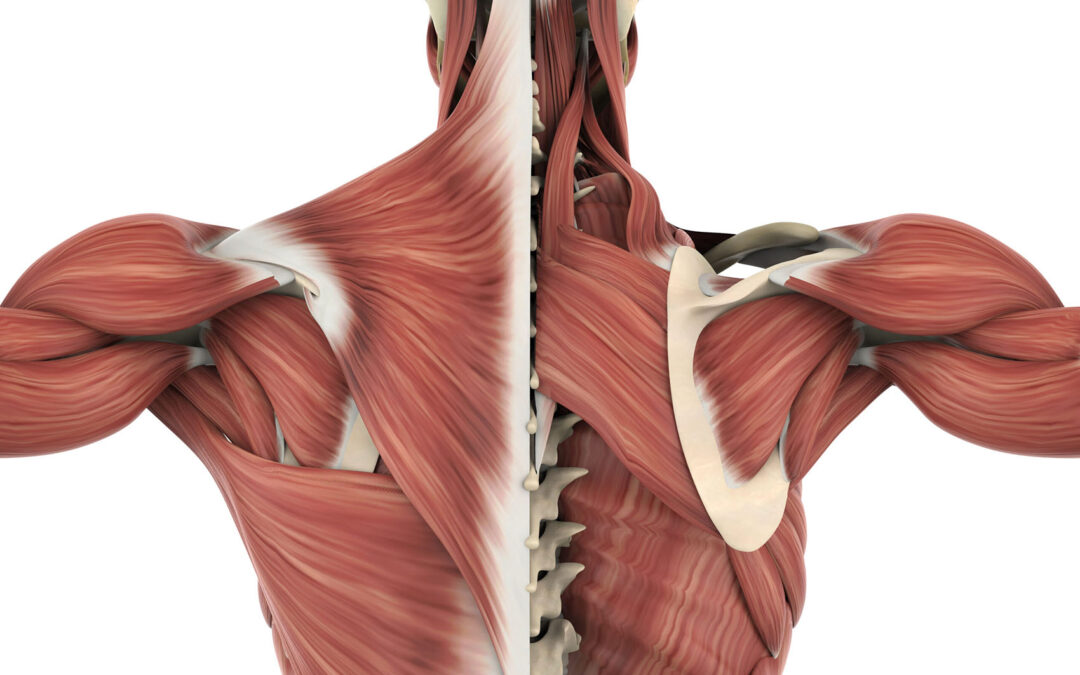
C. New Perspectives: Structural Basis of meridians
1. CT and MRI reconstructions demonstrate structures aligning with expected meridian locations
2. Fascia= extends into interior of the cell
a) many names, same continuous structure
1) perimysium=muscle, perineurium=nerve, periosteum=bone
b) tendons, ligaments, entheses
c) larger structures like plantar fascia, IT band
3. muscle meridians:
a) even now understood that thoracodorsal fascia connects lat dorsi and opposite glute
b) spiral line
c) back functional line
d) front functional line
4. This goes even further: microtubules, cytoskeleton in functions
5. ‘liquid crystal’…piezo-electric effect= deform crystal= electron emission
IV. Light: photons
A. in physics photons are described as
B. fascial network like a fiber optic network
C.extensive fascial system = surrounds and permeates into every cell
V. Big Picture
when we adjust as DC’s we not only move the bones, but we change the forces on the fascial system
when we do massage, ultrasound, trigger point therapy we reduce strain in this system
we are not only normalizing neurologic input, but also the flow of Qi.
VI. It really does come back to chiropractic restoring the flow of vital life force.
VII. We can greatly augment this restoration with acupuncture
trigger points
A. study= approx 70% of TP’s identified were acu points
B. known effects of needle insertion into TP’s
C. Ah-Shi points
D. common formulary points: LI4 for HA, ST 36 for knee pain, etc
E. The explanation
VII. TCM
A. There is a flow of energy through our body that needs to move in a balanced manner for our bodies to be healthy and to heal.
B. Acupuncture (and herbs, if you use them) helps to balance this flow of energy
Westernized
C. Chemical are released at the site of insertion that help to reduce pain, and reduce inflammation in the area.
D. “This then triggers a domino effect of positive changes that assist in healing and calming the irritated nervous system down.”
E. Both are true.
F. Use whichever resonates with you the most
Acupuncture with a Musculoskeletal Focus
I. Acupuncture traditional applications:
A.Cookbook,
B. 5 element theory
1. Wood, Fire, Earth, Metal, Water
2. Traditional Chinese diagnostics: pulse, tongue, etc
C. Ah Shi (AHH-SHIR)
1. Translates as: Yes, there! Ouch, there it is!
2. simply put, palpate painful points and needle them
3. expand this idea to trigger points and injuries
II. This broader interpretation of Ah Shi in everyday practice
A. Trigger points:
1. typically thought of as the following, or similar: a hyper-irritable spot within a taut band of muscle that is painful on compression, stretch, overload, or contraction of the tissue which usually responds with a referred pain that is perceived distant from the spot.
2. Travel and Simons defined
3. Pain arising from altered nociception = labelled now as “nociplastic pain” by the International Association for the Study of Pain.
4. Central nervous system sensitization
5. In such pain conditions it remains to be elucidated whether TrPs represent symptoms of central nervous system sensitization (consequence of), or contribute to its process.
B. There is some evidence from studies supporting that TrPs can be a peripheral source of nociception, and may act as ongoing nociceptive stimuli contributing to pain propagation and central sensitization, and treatment reduces central sensitization.
C. Also evidence suggesting that central sensitization can also promote TrP activity, creating a bidirectional interaction.
III. A remarkably high degree (71%) of correspondence was found. This close correlation suggests that trigger points and acupuncture points for pain
From a neurophysiological viewpoint, treatment may reduce both peripheral and central sensitization
IV. It is known that the insertion of a needle into the body elicits different natural neurophysiological mechanisms like stimulation of the Aδ and C fibers or activation of cortical brain area
V. This idea of bidirectional TPI-brain and brain-TPI is like needling a distal point
needle affecting a central organ = our discussion on fascia and meridians
Using acu on TP’s results not only in pain relief, but a balancing of Qi in the meridian.
VI. Injury
A.Muscle Injury
1. musculotendon junction is the most common place where muscle injury occurs = weakest part
a) acute: MVA, hamstring pull running, biceps avulsion
b) chronic: plantar fascia, tennis elbow, biceps tendonitis
B. tendon injury
C. ligament injury
D. OA
E. wound: circle the dragon
VII. Ah Shi can instill confidence in you
A. Never underestimate the power of the patient’s mind
B. when you touch an area and it hurts and you needle it their confidence in you understanding their condition and that you can help them goes up drastically.
C. We know these using Ah-Shi points symptomatically improve out patients, whether it is TP’s, or at the site of injury as discussed. Let’s consider why for a minute.
D. Assume the fascial basis for the structure of the meridian = when the is damage in an area that the normal flow of Qi thorugh that area cannot go as easily.
E.This is also a very chiropractic concept: proper spinal alignment = proper organ function and improved overall wellness.
VIII. Think of all the things we are up against that cause MSK strain
A.posture:
1. 90% of energy
2. subocc, upper traps, levator; shortened psoas (kidney), pecs, chest expansion reduced
3. think not only of the restrictions in the fascial system this creates as the inner and outer meridians connect but also the mechanical strain on the organs.
B. stress: cortisol’s many affects on body
C. nutrient deficiency
D. toxicity
E. chronic under-hydration
F. all of these things lead to increased sympathetic nervous system tone (HR, BP, sweating), muscle spasm, tightening/shortening of the fascia
G. chronic subluxation and disruption of Qi balance/flow
H. patients need us, b/c no one else is telling them these things.
they need DC, hydration, supplements, good/whole foods, posture improvement, maybe yoga, tai chi, meditation
I. But those of us that have acupuncture to add to those options are doing our patients a great service…synergy: the more they do together the better the results
I. Acupuncture with a Musculoskeletal Focus
1.Simons DG, Travell JG, Simons LS. Travell & Simons’s myofascial pain and dysfunction: the trigger point manual. vol 1 2nd edn Baltimore: Williams & Wilkins, 1999 [Google Scholar]
2. Lavelle ED, Lavelle W, Smith HS. Myofascial trigger points. Anesthesiol Clin 2007;25:841–51 [PubMed] [Google Scholar]
3. Cummings M. Regional myofascial pain: diagnosis and management. Best Pract Res Clin Rheumatol 2007;21:367–87 [PubMed] [Google Scholar]
4. Skootsky SA, Jaeger B, Oye RK. Prevalence of myofascial pain in general internal medicine practice. West J Med 1989;151:157–60 [PMC free article] [PubMed] [Google Scholar]
5. Simons DG. New aspects of myofascial trigger points: etiological and clinical. J Musculoskelet Pain 2004;12:15–21 [Google Scholar]
6. Chang CW, Chang KY, Chen YR, et al. Electrophysiologic evidence of spinal accessory neuropathy in patients with cervical myofascial pain syndrome. Arch Phys Med Rehabil 2011;92:935–40 [PubMed] [Google Scholar]
7. Simons DG, Travell JG, Simons L. Myofascial Pain and Dysfunction. The Trigger Point Manual. 3th ed. Philadelphia: Wolters Kluwer; 2019. [Google Scholar]
8. Fernández-de-Las-Peñas C, Dommerholt J. International consensus on diagnostic criteria and clinical considerations of myofascial trigger points: a Delphi study. Pain Med. 2018;19:142–150. doi: 10.1093/pm/pnx207 [PubMed] [CrossRef] [Google Scholar] Palacios-Ceña M, Castaldo M, Wang K, et al. Relationship of active trigger points with related disability and anxiety in people with tension-type headache. Medicine. 2017;96:e6548. doi: 10.1097/MD.0000000000006548 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
9. Ferracini GN, Florencio LL, Dach F, et al. Myofascial trigger points and migraine-related disability in women with episodic and chronic migraine. Clin J Pain. 2017;33:109–115. doi: 10.1097/AJP.0000000000000387 [PubMed] [CrossRef] [Google Scholar] 10. Fernández-de-Las-Peñas C, Galán-del-Río F, Alonso-Blanco C, Jiménez-García R, Arendt-Nielsen L, Svensson P. Referred pain from muscle trigger points in the masticatory and neck-shoulder musculature in women with temporomandibular disorders. J Pain. 2010;11:1295–1304. doi: 10.1016/j.jpain.2010.03.005 [PubMed] [CrossRef] [Google Scholar]
10. Cerezo-Téllez E, Torres-Lacomba M, Mayoral-Del Moral O, Sánchez-Sánchez B, Dommerholt J, Gutiérrez-Ortega C. Prevalence of myofascial pain syndrome in chronic non -specific neck pain: a population-based cross-sectional descriptive study. Pain Med. 2016;17:2369–2377. doi: 10.1093/pm/pnw114 [PubMed] [CrossRef] [Google Scholar]
11. Fernández-Pérez A, Villaverde-Gutiérrez C, Mora-Sánchez A, Alonso-Blanco C, Sterling M, Fernández-de-Las-Peñas C. Muscle trigger points, pressure pain threshold, and cervical range of motion in patients with high level of disability related to acute whiplash injury. J Orthop Sports Phys Ther. 2012;42:634–641. doi: 10.2519/jospt.2012.4117 [PubMed] [CrossRef] [Google Scholar]
12. Bron C, Dommerholt J, Stegenga B, Wensing M, Oostendorp RA. High prevalence of shoulder girdle muscles with myofascial trigger points in patients with shoulder pain. BMC Musculoskelet Disord. 2011;12:139. doi: 10.1186/1471-2474-12-181 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
13. Fernández-Carnero J, Fernández-de-Las-Peñas C, de la Llave-Rincón AI, Ge HY, Arendt-Nielsen L. Prevalence of and referred pain from myofascial trigger points in the forearm muscles in patients with lateral epicondylalgia. Clin J Pain. 2007;23(4):353–360. doi: 10.1097/AJP.0b013e31803b3785 [PubMed] [CrossRef] [Google Scholar]
14. Iglesias-González JJ, Muñoz-García MT, Rodrigues-de-Souza DP, Alburquerque-Sendín F, Fernández-de-Las-Peñas C. Myofascial trigger points, pain, disability, and sleep quality in patients with chronic nonspecific low back pain. Pain Med. 2013;14:1964–1970. doi: 10.1111/pme.12224 [PubMed] [CrossRef] [Google Scholar]
15. Chiarotto A, Clijsen R, Fernandez-de-Las-Peñas C, Barbero M. Prevalence of myofascial trigger points in spinal disorders: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2016;97:316–337. doi: 10.1016/j.apmr.2015.09.021 [PubMed] [CrossRef] [Google Scholar]
16. Meleger AL, Krivickas LS. Neck and back pain: musculoskeletal disorders. Neurol Clin 2007;25:419–38 [PubMed] [Google Scholar]
17. Luime JJ, Koes BW, Hendriksen IJ, et al. Prevalence and incidence of shoulder pain in general population: a systematic review. Scand J Rheumatol 2004;33:73–81 [PubMed] [Google Scholar]
18. Simons DG. Review of enigmatic MTrPs as a common cause of enigmatic musculoskeletal pain and dysfunction. J Electromyogr Kinesiol 2004;14:95–107 [PubMed] [Google Scholar]
19. Hong CZ, Simons DG. Pathophysiologic mechanisms of myofacial trigger points. Arch Phys Med Rehabil 1998;79:863–72 [PubMed] [Google Scholar]
20. Kosek E, Cohen M, Baron R, et al. Do we need a third mechanistic descriptor for chronic pain states? Pain. 2016;157:1382–1386. doi: 10.1097/j.pain.0000000000000507 [PubMed] [CrossRef] [Google Scholar] [Ref list]
21. Fernández-de-Las-Peñas C, Nijs J. Trigger point dry needling for the treatment of myofascial pain syndrome: current perspectives within a pain neuroscience paradigm. J Pain Res. 2019 Jun 18;12:1899-1911. doi: 10.2147/JPR.S154728. PMID: 31354339; PMCID: PMC6590623.
22. Butts R, Dunning J, Perreault T, Mourad F, Grubb M. Peripheral and spinal mechanisms of pain and dry needling mediated analgesia: A clinical resource guide for health care professionals. Int J Phys Med Rehabil. 2016;4:2. doi: 10.4172/2329-9096.1000327 [CrossRef] [Google Scholar] Melzack R, Stillwell DM, Fox EJ. Trigger points and acupuncture points for pain: correlations and implications. Pain. 1977 Feb;3(1):3-23. doi: 10.1016/0304-3959(77)90032-X. PMID: 69288.
23. Wang CC, Huang TH, Chiou KC, Chang ZY. Therapeutic Effect of Superficial Acupuncture in Treating Myofascial Pain of the Upper Trapezius Muscle: A Randomized Controlled Trial. Evid Based Complement Alternat Med. 2018 Dec 2;2018:9125746. doi: 10.1155/2018/9125746. PMID: 30622617; PMCID: PMC6304674.
II. Acupuncture: Structural Meridian Concepts
1. Bai Y, Wang J, Wu JP, Dai JX, Sha O, Tai Wai Yew D, Yuan L, Liang QN. Review of evidence suggesting that the fascia network could be the anatomical basis for acupoints and meridians in the human body. Evid Based Complement Alternat Med. 2011;2011:260510. doi: 10.1155/2011/260510. Epub 2011 Apr 26. PMID: 21584283; PMCID: PMC3092510.
2. Oschman, J.L, Energy Medicine: The Scientific Basis, 2nd Ed., Churchill Livingstone, 2016
3. Ling, G., N., Life at the Cell and Below-Cell Level: The Hidden History of a Fundamental Revolution in Biology, Pacific Press, New York, 2001
4. Ho, Mae-Wan, The Rainbow and the Worm: The Physics of Organisms, 2nd Edition, Open University, UK, August, 1998, https://doi.org/10.1142/3750
5. D. Damjanovic, Encyclopedia of Condensed Matter Physics: Piezoelectricity, 2005
6. Pagliaro G (2020) A case study of photon detection after acupuncture stimulation Trends Med, 2020 doi: 10.15761/TiM.1000240
7. Hu X, Wu B, Wang P (1993) Displaying of meridian courses travelling over human body surface under natural conditions. Zhen ci Yan Jiu 18: 83-89.
8. Kwang-Sup S (2003) Bonghan duct and acupuncture meridian as optical channel of biophoton. Journal of the Korean Physical Society 45: 1196-1198.
9. Slawinski J, Gorski Z (2008) Imaging of biophoton emission from electrostimulated skin acupuncture point jg4: Effect of light enhancers. Indian Journal of Experimental Biology 46: 340-344.
10. Hobbs R (2009) The biophysics of acupuncture: emerging patterns from selected studies. Medical Acupuncture 21. Chen GZ, Xu YX, Wang YH, Yang HQ, Lin QY, et al. (2011) Optical transport properties along the pericardium meridian under different pressure. J Lasers Med Sci 2: 89-97.
11. Li N, Guo Y, Gong Y, Zhang Y, Fan W, Yao K, Chen Z, Dou B, Lin X, Chen B, Chen Z, Xu Z, Lyu Z. The Anti-Inflammatory Actions and Mechanisms of Acupuncture from Acupoint to Target Organs via Neuro-Immune Regulation. J Inflamm Res. 2021 Dec 21;14:7191-7224. doi: 10.2147/JIR.S341581. PMID: 34992414; PMCID: PMC8710088.
Kyle Hagel, DC
Dr. Hagel has over 20 years of practice experience with a diverse practice background that includes Evaluation and Management of Auto Injuries, Functional Muscle Evaluation, Sports Medicine, Postural Reeducation, Structural Correction, Disc Injury Management, Spine and Extremity Bracing, Neuropathy Pain Management, Weight Loss, Functional Medicine, and Acupuncture. He also has benefitted greatly from working cooperatively with Physicians, Physician Assistants, and Nurse Practitioners in an integrated clinic for the last 14 years and continues to do so.
Educating patients has always been very important to Dr. Hagel in his practice. Patients that understand their condition make better decisions about their care. He is excited to now be involved in chiropractic continuing education and helping other doctors to do the same for their patients.